In 1972, historian Alfred Crosby introduced the term Columbian Exchange to refer to the interchange of plants, animals, bacteria, and peoples that occurred between the Old World (Eurasia and Africa) and the New World (the Americas and Australia) following the arrival of Christopher Columbus in the Americas in 1492. One of the most profound and far-reaching effects of that exchange concerned microorganisms and the diseases they caused.
In the Old World, epidemic crowd diseases had evolved along with the earliest civilizations, but they had no equivalents in the New World. When the new diseases spread to the Americas and to peoples who had never experienced them before, the results were dramatic and sometimes catastrophic. The interhemispheric disease exchange resulted in what has been called the "greatest demographic disaster in human history." Millions died.
The list of diseases introduced to the New World is long, and nearly all that could be supported in a temperate environment appeared in present-day Oregon. The most deadly were smallpox, malaria, viral influenza, yellow fever, measles, typhus, bubonic plague, typhoid fever, cholera, and pertussis (whooping cough). Among these, half appeared in epidemic form in Oregon during the first century of encounters between Natives and non-Natives, from the late 1700s through the mid-1800s.
It has been hypothesized that Oregon and the West Coast participated in the first great pandemic of introduced epidemic disease—smallpox in 1519 and the years following (introduced to the mainland concurrent with Cortez's conquest of Mexico)—but there is no definitive proof of this anywhere in the Northwest. Whenever the first epidemics appeared, they had wide-ranging effects far beyond demographic decline. Cumulative evidence suggests that cultural unfamiliarity with the new diseases—that is, people did not know how to treat them—and the lack of effective medicines may have been as or more important than biological resistance, genetic or acquired, in accounting for the high mortalities. The loss of population resulted in abandoned and consolidated villages, the breakdown of social and political structures, and the loss of cumulated knowledge possessed by specialists (in a culture without written records), making the epidemics cultural as well as biological disasters.
Smallpox
The earliest documented epidemic in Oregon was smallpox. The year was most likely 1781, the date of a major epidemic throughout North America east of the Rockies, though this has been hard to pin down because most estimates come from after-the-fact observations by white explorers of pockmarked individuals. An oral tradition from the Clatsop of a shipwreck and the introduction of a spotted disease, however, dates to a decade before Robert Gray entered the Columbia in 1792, providing a close fit with the timing of the East Coast epidemic.
The epidemic probably occurred throughout the Pacific Northwest. There are records in oral traditions or from white explorers of pockmarked individuals among the Tlingit, Haida, Tsimshian, Kwakwakawakw (Kwakiutl), Nuuchahnulth (Nootka), Lummi, Puget Salish, Tillamook, Colville, Flathead, and Nez Perce. The epidemiology of smallpox—spread easily by a sneeze or through touch—predisposed that it would spread rapidly and thoroughly among concentrated populations and by flight from one community to another. The journals of the Lewis and Clark Expedition describe two instances of pockmarked people in Oregon, one from Clatsop and one from a Chinookan village near the Sandy River. William Clark wrote: "they all died with the disorder...Small Pox destroyed their nation."
We do not know how many people died in the first epidemic, but the records suggest it was large. Virgin soil (that is, first-time) smallpox epidemics generally claim an average of 30 percent of the population, but that figure may be conservative. By the time Robert Gray entered the Columbia in 1792 and non-Native fur traders began frequenting the Oregon Coast, Native populations were already depleted and their cultures were damaged.
Smallpox either kills infected individuals or, if they survive, leaves them with an acquired immunity to later outbreaks. There were more smallpox epidemics in the Pacific Northwest, and their timing—1800-1801, 1824, 1836, 1853, and 1863—suggests that the disease recurred whenever there was a sufficiently large cohort of nonimmune people who had been born since the last outbreak and were, hence, vulnerable to infection. In Oregon, both the 1800-1801 and 1824 epidemics are documented, but neither seems to have been as severe as the epidemic of the late 1700s. The 1836 epidemic is not recorded for Oregon other than in the southwest quadrant, and the 1863 epidemic was limited to British Columbia and Alaska. The 1853 epidemic, however, struck people throughout the lower Columbia, claiming half of the Native communities at Chinook and The Dalles. By 1853, smallpox vaccine was available in Oregon, but it did not reach the Indians.
Malaria
Malaria occurred in annual outbreaks starting in 1830 and was most intense in its effects until 1834. The disease clearly claimed a large proportion of the Native population and may have exceeded in numbers the deaths from the first smallpox epidemic. There has been some controversy over the identity of the epidemic of the 1830s, given that it died out and that the symptoms and terminology assigned to it were not often clear. Studying the epidemiology of the disease, however, makes clear that it was malaria, which is caused by a protozoan that enters the bloodstream with a bite from an infected Anopheline mosquito. Although the insect is rare in Oregon today, a potential vector, Anopheles freeborni, was common in western Oregon until the early 1900s. In Oregon, Anophelines breed and bite during the summer, and that is when the epidemics recurred. Native Anophelines favor low-lying swampy areas and do not breed in high elevations or brackish water near the coast, and that matches the range of the 1830s outbreaks.
Malarial symptoms are variable, but the most pronounced are the regular spells of fever and cold, which are recorded time after time for the 1830s epidemic. The word malaria had not yet been coined by 1830, but alternate names refer to the symptoms—“fever and ague” and “intermittent fever.” The medicine used until recently to treat malaria—quinine, from the bark of the cincona tree—was used to treat the 1830s Oregon epidemic, although supplies were few.
Fever and ague appeared suddenly in July 1830 in Native villages on and around Sauvie Island near Fort Vancouver. The Indians believed it had been introduced by an American ship involved in the salmon trade, the Owyhee, commanded by John Dominis. They may have been right, as the ship had visited malarial ports before sailing to the Columbia. As the epidemic broke out simultaneously in the villages and at the fort, Hudson's Bay Company (HBC) personnel were kept busy and did not witness what happened in the villages. Only later, when Peter Skene Ogden visited Sauvie Island, did the destruction become clear. Because of their proximity to dense mosquito breeding areas and the counterproductive effect of treating the fever attacks by plunging into cold water, high mortalities in villages were assured. At the fort, cases continued to be reported until November; but because the HBC had quinine and knew how to treat the spells of heat and cold, deaths among whites were few.
In 1831, 1832, and 1833, fever and ague reappeared each summer, claiming more people every year and in a widening geographic focus. Chief Concomly of the Chinooks, who was probably infected on a trip upriver, died in 1830. In 1831, the epidemic extended into the Willamette Valley and up the Columbia River Gorge. By the next year, it was probably in southern Oregon. In all these places, the demographic results were nothing short of apocalyptic. Comparing Lewis and Clark's estimates of population in the Portland Basin with numbers from the late 1830s, an estimated 90 percent of the people died. Similar statistics from the Willamette Valley show a loss in the 80 percent range.
The impact of fever and ague on Native people in Oregon was earthshaking. In the 1820s, they had been by far the majority population in the region; by the early 1840s, they were in the minority. Villages were abandoned, and Native cemeteries overflowed. The Willamette Mission in present-day Salem started its Indian school in 1835 with orphans. What white settlers rarely saw or recorded was the anguish of the survivors, the social breakdown, and the cultural loss that affected Native communities in those terrible years. The 1830s epidemic had effects that have remained with Oregon Indians to this day.
Measles
There were other less deadly epidemics of introduced diseases during the first century of enconters between Natives and non-Natives: influenza in 1836; a dysentery epidemic that was probably shigellosis, introduced from the South Seas to the lower Columbia in 1844; and the 1853 smallpox epidemic. But demographically, culturally, and politically, the next most important introduced disease in Oregon was the measles epidemic of 1847-1848. Measles was possibly present earlier (the 1824 epidemic may have been measles, not smallpox), but in all other ways the 1847 epidemic played out like a virgin-soil visitation. A significant percentage of the affected Native population—set at 10 percent by HBC Chief Factor James Douglas—died from the disease.
Measles was not initially introduced to Oregon by settlers on the Oregon Trail, although they picked it up on the trail near Walla Walla and spread it further. It came instead from the California central valleys, carried north by a party of mounted mid Columbia Indians who had been to the area near Sutter's Mill to acquire Mexican cattle. They returned to Fort Nez Perces (present-day Walla Walla) mourning the loss of members of their party to measles, and it appears that the remainder of the group dispersed and carried the disease to their home villages.
By early November, deaths—concentrated among children—were occurring almost daily at the Cayuse village near Waiilatpu Mission, and the chiefs, perhaps prodded by Natives from elsewhere, suspected that Marcus Whitman may have caused the disease. Because Natives assumed that powerful medicine men could not only cure but also cause disease, the theory fit their beliefs. For them, removing the cause of the disease was the only logical response, and that was part of the reason for killing the Whitmans.
The measles epidemic spread through both white and Native intermediaries west, southwest, and north from the area around Walla Walla. Immigrants carried it along the last stretch of the Oregon Trail to Fort Vancouver and Oregon City, and from there to the diminished Native communities in the Willamette Valley. It also spread throughout Washington and British Columbia, carried to the north coast of British Columbia by the Hudson's Bay Company vessel, the Beaver.
The last important epidemic of introduced disease to affect Oregon Natives was smallpox in 1853. By the late 1850s, most Indians had been removed to reservations, and different diseases, mostly chronic, took hold. Tuberculosis, which was especially severe among the Nez Perce, and trachoma became prevalent on Oregon reservations in the late nineteenth and early twentieth centuries. Tuberculosis may or may not qualify as an introduced disease, since similar mycobacterial diseases are known from the time before encounters between Natives and non-Natives in North America.
In the twenty-first century, though there are differences, all Oregonians share essentially the same pool of diseases. Many of them, however, are not native to the state and were introduced by non-Natives with tragic consequences for Native peoples.
-
![]()
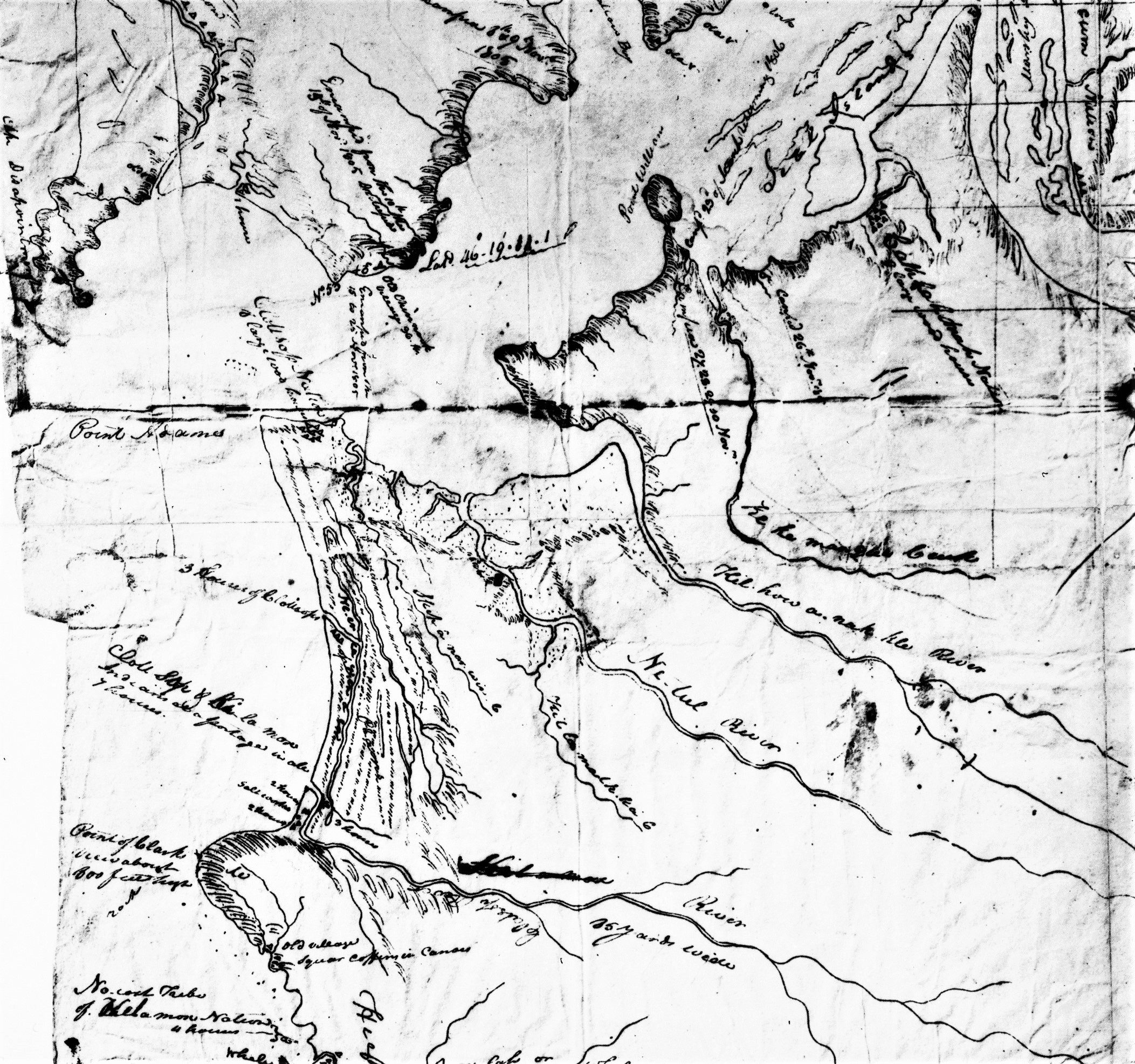
Section of Lewis and Clark's 1806 map of the lower Columbia, showing Pt. Adams and the Clatsop village Neak'ilaki; the future site of Indian Place is south along the coast, labeled "Clott Sopp and Ki la mox.".
Courtesy Oregon Hist. Society Research Lib., bb010758
-
![]()
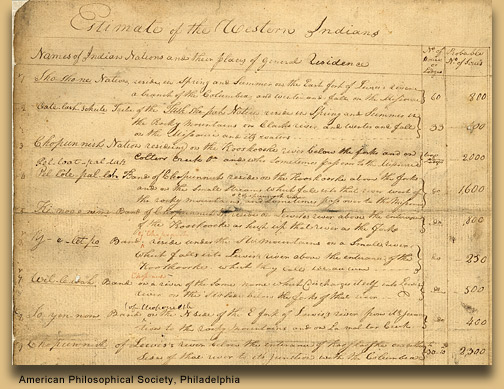
Estimate of Western Indians, Lewis and Clark.
Courtesy American Philosophy Association, Philadelphia
Related Entries
-
![Cathlapotle]()
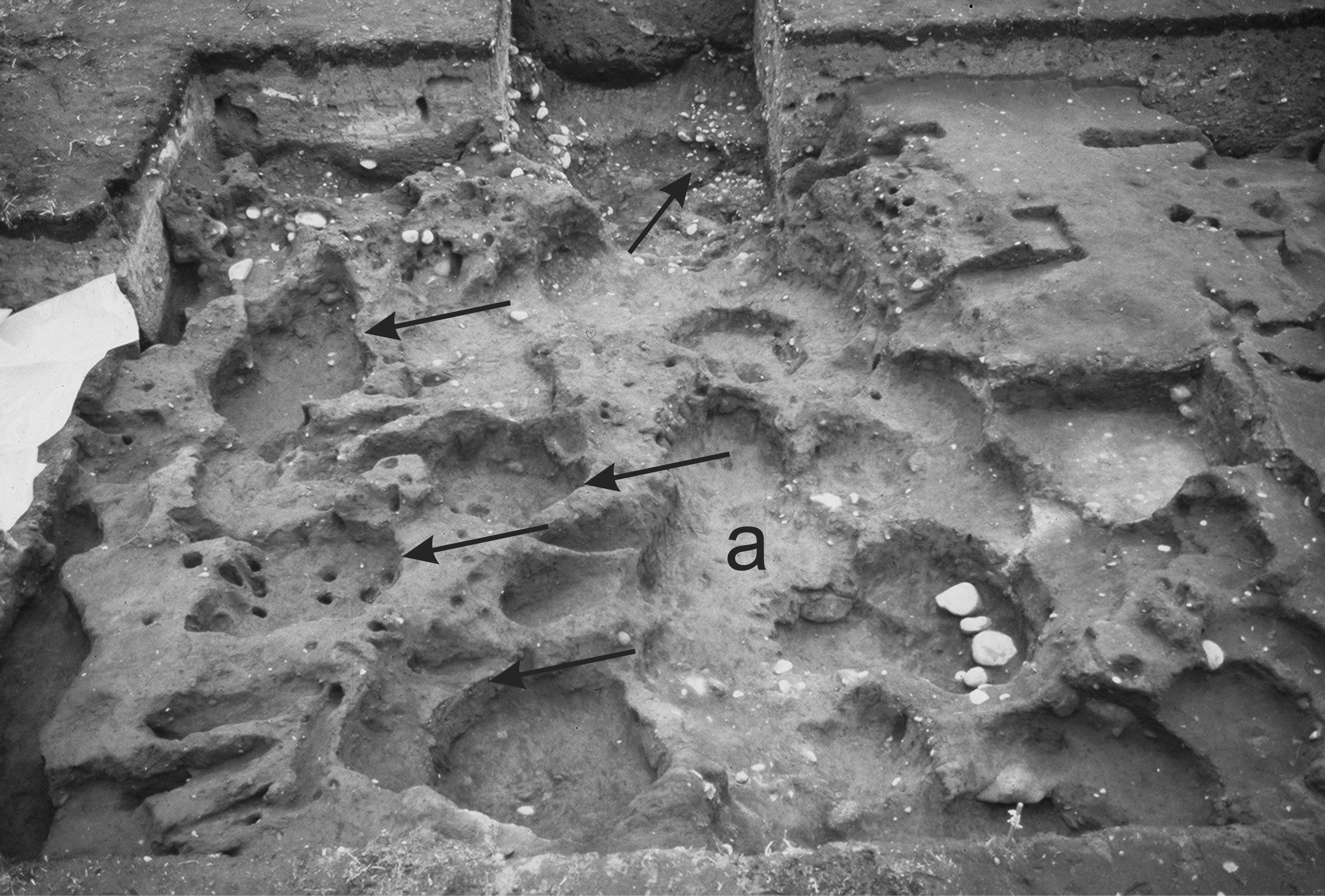
Cathlapotle
Cathlapotle is the archaeological site of a major Chinookan town locate…
-
![Confederated Tribes of Grand Ronde]()
Confederated Tribes of Grand Ronde
The Confederated Tribes of Grand Ronde Community of Oregon is a confede…
-
![Kalapuyan peoples]()
Kalapuyan peoples
The name Kalapuya (kǎlə poo´ yu), also appearing in the modern geograph…
-
![Meier Site]()
Meier Site
The Meier site, the subject of an archaeological excavation that docume…
-
![Wapato (Wappato) Valley Indians]()
Wapato (Wappato) Valley Indians
Lewis and Clark called them the "Wappato Indians," the people who inhab…
Related Historical Records
Map This on the Oregon History WayFinder
The Oregon History Wayfinder is an interactive map that identifies significant places, people, and events in Oregon history.
Further Reading
Boyd, Robert. "Another Look at the 'Fever and Ague' of Western Oregon." Ethnohistory 22.2 (1975): 135-54.
Boyd, Robert. "Demographic History, 1774-1874." In Wayne Suttles (ed.) Handbook of North American Indians, vol. 7, Northwest Coast, 135-48. Washington, D.C.: Smithsonian Institution, 1990.
Boyd, Robert. "The Pacific Northwest Measles Epidemic of 1847-1848." Oregon Historical Quarterly 95.1 (1994): 6-47.
Boyd, Robert. The Coming of the Spirit of Pestilence: introduced infectiouus diseases and population decline among Northwest Coast Indians, 1774-1874. Seattle and Vancouver: University of Washington and UBC Presses, 1999.
Boyd, Robert. "Lower Chinookan Disease and Demography." In Chinookan Peoples of the Lower Columbia, edited by Robert Boyd, Kenneth Ames, and Tony Johnson. Seattle: University of Washington Press, 2013.
Campbell, Sarah." Postcolumbian Culture History in the Northern Columbia Plateau, A.D. 1500-1900." PhD diss., University of Washington, 1989.
Cook, Sherburne. "The Epidemic of 1830-33 in California and Oregon." University of California Publications in American Archaeology and Ethnology 43.3 (1955): 303-26.
Crosby, Alfred. The Columbia Exchange: biological and cultural consequences of 1492. Westport, Conn.: Greenwood, 1972.
Fenn, Elizabeth. Pox Americana: the great smallpox epidemic of 1775-82. New York: Hill and Wang, 2001.
Heizer, Robert. "Walla Walla Expeditions to the Sacramento Valley." California Historical Quarterly 23.1 (1942): 1-7.
Lewis, Meriwether and William Clark. The Journals of the Lewis & Clark Expedition vol. 7, March 23, 1806-June 9, 1806. Edited by Gary Moulton. Lincoln: University of Nebraska Press, 1991.